The triangular relationship between modern psychiatry, pharmaceutical companies, and the people who get diagnosed with mental illness is probably one of the more contentious in medicine, especially in the eyes of the public. The re-framing of mental illness, especially depression, as a “chemical imbalance” was at once a pharmaceutical marketing trick and something that some patients felt powerfully reduced stigma and guilt of having a diagnosis. Psychiatrists are rated below other medical specialties in public polls identifying the most trustworthy professions, though they’re still in the top 10.
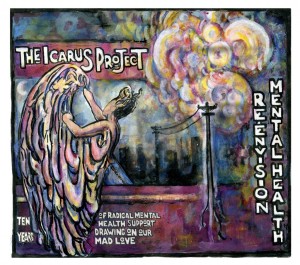
Peer support for patients outside of mainstream medicine exists has sprung up in groups like the Icarus Project, which claims to be “navigating the space between brilliance and madness” and conceptualizes mental illness not as diseased state that must be cured, but as a “dangerous gift.” I have mixed feelings of discomfort and excitement at that idea, which may be biased by my own personal negative encounters with local people in a related group. Perhaps it depends on the consequences of such a construction. Does it empower patients (or certain subsets of patients) and help them feel they are valued members of society and get them back to being capable of doing what they want to do with their lives? If so, great! That’s the ultimate goal of medical treatment – to restore function and the ability to live to a person who may have been incapacitated by their psychiatric condition. But restoring function is kind of a tricky thing to define here. It’s not the same as operating on a broken bone – function restored! What if people are able to go back to work after being out on disability for mental illness but are traumatized from what they experienced, say, on an inpatient psychiatric ward? What if some fundamental shift occurs because they now have a history of psychiatric hospitalization, not just through external stigma, but due to internalization of the fact that they are diseased? I don’t think any doctor wants that, but it may be hard for doctors to know if they’re having this effect.
I just completed an unpublished memoir written by a man who has Bipolar I disorder. This is the most serious form, characterized by alternating episodes of elevated and depressed mood, or as the author describes, “You have mania, depression, then something else that’s neither mania nor depression but something new that’s the result of mania and depression having been there.” Maybe memoir doesn’t quite capture it all – it was at once the story of his experience with Bipolar disorder, a critique of his American psychiatric treatment, some radical Christian theology, all mixed with an impressive dose of self-awareness.
He writes about the phenomenon of becoming a person who is undergoing psychiatric treatment, “He will become no longer someone to whom something strange is happening. He will become that something strange.”
Before I discuss the content of his book more and reflect on lessons I took from it, I want to provide some background about my experience with psychiatry and mental illness. I’ve had a longstanding interest in psychiatry; when I entered medical school, I was certain I was going to choose that as a specialty. I envisioned it to be very fulfilling to be able to respond to a person who is suffering, comfort them, and contribute to the restoration of their function and pursuit of a meaningful life. I was interested in how new research from neuroscience and positive psychology might inform the field and improve treatment. I have many thoughts and questions about how doctors in training are taught to conceptualize mental illness, what the patients’ experiences are like, and how a good psychiatrist or primary care doctor would treat these patients. (Actually, after reading the memoir, I have feel less comfortable using terms like “patient” when applied to an otherwise healthy person with a primarily psychiatric issue. We’ll just keep it for simplicity for the time being.)
My own experience during my psych rotation was pretty similar to what I expected from prior reading. Psychiatrists, like the vast majority of doctors, deeply care about their patients and want to help them get better. The most widely accepted theory of illness, especially mental illness, and approach to treatment is the biopsychosocial model – the theory that an individual’s biological/genetic make-up, thoughts/beliefs, and environment all interact to promote disease (or protect against it).
We were taught that maintaining boundaries is more important in psychiatry than other specialties, because overstepping these can be coercive or confusing to a patient. Psychiatrists don’t touch their patients much, if at all. Curiously, in other fields, patients often feel dissatisfied if they are not physically examined by the doctor. “The laying on of hands can be therapeutic and builds rapport,” according to the Tarascon Emergency Department Quick Reference Guide. Instead, the mental status exam and clinical interview are the most important assessment tools for psychiatrists.
Reading his memoir reaffirmed that mental illness is dramatically different from other types of illness, despite our brains (and the things that go wrong with them) being part of our bodies. There is absolutely no question that the author has been diagnosed with Bipolar I and was manic (or at least hypomanic) when he wrote the piece. His writing at times demonstrates some pretty classic symptoms of formal thought disorder that people can exhibit during manic episodes – loosening of associations, flight of ideas, stilted speech at times, tangentiality, even some ideas of reference.
It’s not hard for me to imagine him trying to tell his story and ideas to a busy psychiatrist, with the doctor all the while checking off symptoms and maybe writing some notes, but completely missing the point of what he was trying to convey. Maybe a doctor casually mentioned “you should write a book.”
The main criticism of American psychiatry is nicely summarized early on:
“We are radically connected to each other, and radically loved. When we fully validate each other, validating each other’s humanity, we are redeemed from the separation that causes us to a) lose hope and b) forget who we are…Psychiatry doesn’t fully validate the humanity of the mentally ill. Psychiatry is a product of a society which operates using stigma. Stigma exists where there should be solidarity. Psychiatry misses our radical connectedness with each other.”
What if he’s right? In the realm outside “right” and “wrong,” his experience is his experience, and if he feels that psychiatry doesn’t affirm him as a human first, then he IS right and the specialty has mostly failed him. He is strongly influenced by theology, and while reading, I began to think about how frequently “healthy” people are not only willing to submit to the possibility, but are absolutely certain of the truth of their religion’s teachings, even if they include (and they almost always do) aspects that seem to defy the laws of nature, like Jesus rising from the dead and ascending into heaven. The DSM-IV, psychiatry’s Bible, explicitly states that religious beliefs are not included in the criteria for delusions and hallucinations. It is very obvious and yet very strange to include such a distinction. Many, perhaps most, people very strongly hold beliefs that seem bizarre to people outside of the religion. Does this have any implication for what it means to be mentally ill? I’m not sure.
When I was doing some overnight shifts in the ER on my psych rotation, I was surprised by how bluntly the psych resident asked incredibly personal and complicated questions. “Have you felt that there are ideas or messages out there that are special to you or that only you understand?” or “Have you felt like life is not worth living and you would be better off dead?” and then seem annoyed when the patient broke out into a really detailed story. That’s not something you can really say yes or no to, then shut up, and wait patiently for the next question. But that’s exactly what the resident wanted. Of course, the resident was working busy overnight shifts and was understandably tired. And the primary goal of an ER assessment is to determine if a patient needs admission to the psych unit, whether voluntarily or otherwise. But isn’t there something about that process that could be therapeutic or traumatizing in itself? Again, it’s not the same as working someone up for new chest pain to rule out a myocardial infarction by ordering a panel of tests and basing the decision to admit on their results, but the profession has tried to make the approach similar in psychiatry.
When I’ve spoken to manic or psychotic patients who are explaining a delusion, I have found it tempting to interrupt them to continue the interview, probably for several reasons. To be completely honest, one is that being in the presence of a floridly psychotic person for a long time can make me uncomfortable, and I suspect this isn’t uncommon among doctors. This is something that I wish to work on, personally, but it is the reality of the situation right now. Also, the specific content of their delusions and thought disorder is not the most relevant to diagnosing and determining their treatment plan. For example, it doesn’t really matter if a patient comes in saying he can hear his dead mother and uncle fighting in his head and telling him to do things – what matters is that he is having command auditory hallucinations, which is highly associated with schizophrenia. Regarding the content of the thoughts, distinctions are made between “bizarre” and “non-bizarre” delusions – bizarre is something that could not actually happen, ie., “a device is implanted in my head by the government and projecting my thoughts,” whereas non-bizarre could possibly be true in the real world, ie., “my wife is cheating on me.” There is no discussion among psychiatrists about whether the patient might actually be onto something, or expressing some deep, fundamental, metaphorical truth in their mania. Yet the specific content of the thoughts and not the pattern, is obviously what concerns the patient.
So what we’re actually doing is taking something that is deeply personal and “real” to the patient, and placing it in the appropriate pathological category to come up with a differential diagnosis of diseases, which are by and large patterns of behavior that are fairly consistent in general, but not specific content. Essentially we are listening to them in order to gather specific information, not to meet them, human-to-human, and reflect on the nature of our shared reality. I believe this is what he means when he says, “Your experience is deeply unvalidated . It is devalued. It is pathologized. An experience is so radically unvalidated that it’s (sic) character as an experience is stripped from it.”
Later, he describes what he wants from mental health professionals, “How can I make you understand when I don’t? But if I can show you that crater–if I can detonate a charge that creates a crater–it is conceivable that you might make a place for us, the crazy people, that isn’t based on exclusion and stigma. You might be like, ‘I don’t understand all the details of what you’re saying, but it sure sounds like something was going on. It sure sounds like there’s not just an absence of culture and a lack of sanity but there is more going on in you and the thing is that this means there is more to me than I realized. For I am you and you are me. I have only been so engaged with my life. There’s more that I didn’t realize was there. I’m not going to treat you like you’re weird any more. I’m not going to create a divide between us. Let’s everybody heal.’”
I am very much with him in wanting to understand more about his experiences and what led them to seek treatment (whether of his own accord or not). It was so helpful to hear him describe his symptoms in the context of his entire life. Yet I found myself wondering if this person’s judgment could really be trusted, and how representative of others with bipolar disorder his experience is. Which curiously got me wondering what it means to trust someone’s judgment and how arbitrary the criteria really are.
That’s the thing about people with bipolar disorder. Being around them has always made me fall into some sort of hyper-subjectivity and frame shift which isn’t really embraced by medicine. Medicine increasingly seeks to identify patterns and develop treatment algorithm patterns to implement the “standard of care.” Payment is based on DSM-IV and ICD-10 codes – numbers that represent a disease process, a condition, an experience. After reading this memoir, I can understand how bizarre and unappealing that seems to a manic person, who is at once asserting that he be treated as an individual by medical staff, yet also calling for the recognition that all humanity is bound by a shared experience, and his suffering is our suffering. I don’t think that MUST be necessarily in conflict, but I fully admit I have NO ready solution.
He starts with some very compelling descriptions of his thoughts and his experiences which immediately resonate with me as a person deeply interested in social justice. “Madness is lonely. That’s why I’m writing, to address the deep loneliness of insanity. It’s a source of solace to believe that a solidarity can or might exist. This solidarity would rescue us from the loneliness. This solidarity must be based on the recognition of the full humanity of the madman or woman. It is not just a disease or a demon, it is a person who suffers, just like we all suffer. My suffering is your suffering, and yours is mine. I am radically flawed–so are you. This is the key to our shared humanity and our solidarity. My experience is not mine, and your experience is not yours.” I agree. I don’t think there is anything about modern medicine that is in contradiction to that philosophically, but I no doubt think that the practical treatment of psychotic and manic patients does not really affirm this model.
To say that I was left with more questions than answers is an understatement. I think we should be on the verge of a paradigm shift in how mental illness is conceptualized and treated. But I do not know how that would be possible under our current payment system.